The SOAP Note section provides the breakdown of subjective, objective, assessment, and plan during all four years of Medical School, and Residency. Prepare and Learn Ahead! Educating and providing resources to students interested in the medical field.
Subjective
HPI
- include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient).
| OLDCARTS Onset Location Duration (How long it lasts) Character Association, Aggravation, Alleviation Radiate Timing (Morning, Afternoon, Evening) Severity (from 0-10 scale) | OPQRST Onset Provocation/palliation Quality Region/Radiation Severity Time | CODIERS Chronology Onset Duration Intensity Exacerbation Remitting Symptoms associated |
Past History
- PMH – Pertinent past medical history
- PSH – Pertinent past surgical history
- Hospitalization
- Meds – Current medications (list with daily dosages)
- Allergies – Medication, Food, Seasonal, and Latex
- Screening
- Vaccines
- Current PCP
Family History
- Father – Age, Medical Condition
- Mother – Age, Medical Condition
- Brother – Age, Medical Condition
- Sister – Age, Medical Condition
- Children – Age, Medical Condition
Social History
- Marital Status
- Sexual Preference
- Sexually Active/Partners
- Occupation
- Alcohol consumption
- Tobacco products
- Illicit Drugs
- Food/Diet
- Exercise
ROS
- Const. (Health in General)
- Lack of energy, unexplained weight gain or weight loss, loss of appetite, fever, night sweats, pain in jaws when eating, scalp tenderness, prior diagnosis of cancer.
- Ears, Nose, Mouth & Throat
- Difficulty with hearing, sinus problems, runny nose, post-nasal drip, ringing in ears, mouth sores, loose teeth, ear pain, nosebleeds, sore throat, facial pain or numbness.
- C-V (Heart & Blood Vessels)
- Irregular heartbeat, racing heart, chest pains, swelling of feet or legs, pain in legs with walking.
- Resp. (Lungs & Breathing)
- Shortness of breath, night sweats, prolonged cough, wheezing, sputum production, prior tuberculosis, pleurisy, oxygen at home, coughing up blood, abnormal chest x-ray.
- GI (Stomach & Intestines)
- Heartburn, constipation, intolerance to certain foods, diarrhea, abdominal pain, difficulty swallowing, nausea, vomiting, blood in stools, unexplained change in bowel habits, incontinence.
- GU (Kidney & Bladder)
- Painful urination, frequent urination, urgency, prostate problems, bladder problems, impotence.
- MS (Muscles, Bones, Joints)
- Joint pain, aching muscles, shoulder pain, swelling of joints, joint deformities, back pain.
- Integ. (Skin, Hair & Breast)
- Persistent rash, itching, new skin lesion, change in existing skin lesion, hair loss or increase, breast changes.
- Neurologic (Brain & Nerves)
- Frequent headaches, double vision, weakness, change in sensation, problems with walking or balance, dizziness, tremor, loss of consciousness, uncontrolled motions, episodes of visual loss.
- Psychiatric (Mood & Thinking)
- Insomnia, irritability, depression, anxiety, recurrent bad thoughts, mood swings, hallucinations, compulsions.
- Endocrinologic (Glands)
- Intolerance to heat or cold, menstrual irregularities, frequent hunger/urination/thirst, changes in sex drive.
- Hematologic (Blood/Lymph)
- Easy bleeding, easy bruising, anemia, abnormal blood tests, leukemia, unexplained swollen areas.
- Allergic/Immunologic
- Seasonal allergies, hay fever symptoms, itching, frequent infections, exposure to HIV.
Objective
Vital Signs:
- Temperature is 37.9 C (100.2 F)
- Pulse is 94 beats/minute
- Respiratory rate is 18 breaths/minute
- Blood pressure is 140/70 mmHg
- spO2 is 98 in RA
- Body Mass Index is 21 kg/m2
Physical Exam
- General: Older adult female in no acute distress, sitting in bed.
- ENT: Extraocular eye movements (EOM) intact, dry oral mucous membranes, neck supple, no jugular venous distension (JVD).
- Lungs: Clear to auscultation bilaterally, symmetric expansion and good effort.
- Heart: Regular rate and rhythm, normal S1 and S2 are appreciated. No murmurs, gallops, or rubs.
- Abdomen: Mild tenderness to moderate palpation throughout, no rebound or guarding, hyperactive bowel sounds, no costovertebral angle tenderness.
- Extremities: 2+ pulses throughout, trace edema in ankles bilaterally.
- Neuro: Alert, oriented to person, place, time, and situation. Able to follow directions.
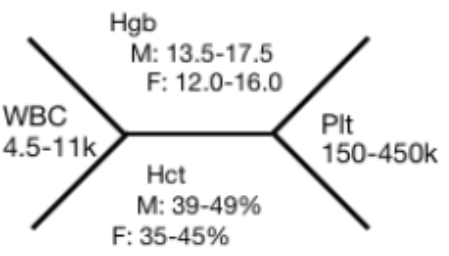
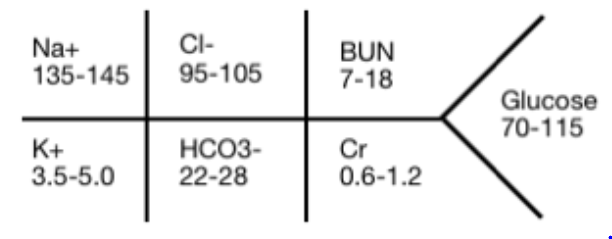
Lab Work
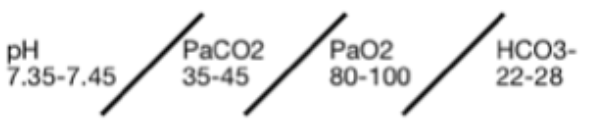
| CBC CMP UA Urine Culture Blood Culture Wound Culture TSH and free T4 Lipid panel Vitamin D level | BNP Troponins x3 CRP ANA panel Hepatitis panel Procalcitonin Lactic acid Ammonia Level Mg and phosphate level |
| ABG pH PCO2 exPCO2 HCO3- AG |
 |  |  |
Radiological Imaging
| EKG X-ray US CT MRI | Gastrografin Barium |
Assessment
VINDICATE
- V – vascular
- I – infection or inflammation
- N – Neoplasm
- D – drugs/toxins, degenerative processes
- I – iatrogenic, idiopathic
- C – congenital/inherited, developmental
- A – autoimmune, allergic, anatomic defects
- T – trauma
- E – endocrine/metabolic, exposures (environmental, occupational)
