Table Of Contents
Differentials
Wheezing
- Wheezing in infants:
- Wheezing in peds 1 to 4:
- New onset wheezing in a toddler:
- Wheezing in peds 5 to 12:
- Wheezing in adolescence:
Apnea of prematurity (AOP)
- Path:
- Presentation:
- Associated:
- Management:
Asthma
- Diagnostic:
- spirometry
- Management:
- A-drenergics (Albuterol)
- S-teroids
- T-heophylline
- H-ydration (IV)
- M-ask (Oxygen)
- A-ntibiotics
- Stepwise therapy, multiple drug classes:
- Inhaled corticosteroids (↓morbidity, unchanged course)
- Leukotriene modifiers ([1] Leukotriene receptor antagonists, [2] leukotriene synthesis inhibitors)
- Long acting beta-2 agonists (Formoterol, Salmeterol)
- Theophylline (becoming outdated)
- Biologics (anti-IgE; Omalizumab)
- Short-acting beta-2 agonists (albuterol)
- Anticholinergics (Ipratropium)
- Oral corticosteroids (avoid prolonged use)
- Trigger Reduction Tactic:
- Viral upper resp. infection
- ↓Exposure; flu vaccine
- Smoke (tobacco, wood)
- Quit smoking (parents and caregivers); alternate heating
- Dust mites
- Bedding encasements and cleaning
- Animal Dander
- Air filters, separation from pets
- Cockroach allergens
- Pesticides, crack sealants
- Indoor Mold
- Cleaners, dehumidifiers
Bronchiolitis
- Path:
- Presentation:
- MC infants < 1Yo
- Course:
- Sign:
- prolonged expiratory phase, wheeze, nasal flaring, suprasternal retractions, air trapping + lung hyper-expansion
- Grunting and cyanosis = severe disease
- Rhinorrhea, pharyngitis, cough, wheezing, rhonchi, rales
- prolonged expiratory phase, wheeze, nasal flaring, suprasternal retractions, air trapping + lung hyper-expansion
- MC Cause: RSV
- Lab Imaging:
Osmosis / CC BY-SA
- Diagnosis:
- Antigen detection assays
- Treatment:
- Immunocompromised patients: use of antivirals (ribavirin) be recommended

X-ray of a child with RSV showing the typical bilateral perihilar
James Heilman, MD / CC BY-SA
Bronchopulmonary dysplasia (BPD)
- Path:
- chronic lung disorder characterized by bronchiolar metaplasia and interstitial fibrosis
- a chronic lung disease that develops in newborns as a consequence of the treatment of IRDS with oxygen and positive pressure ventilation for a primary lung disorder
- Etiology:
- 1) precise cause is unknown
- 2) common factors include:
- a. low gestational age
- b. mechanical ventilation with high airway pressure
- c. high oxygen concentration
- d. history of IRDS
- 2)PMH – premature
- 1) precise cause is unknown
- Presentations:
- cyanosis
- Physical Exam:
- intercostal retractions
- increased respiratory pattern >60/min
- Breath sounds:
- 1) wheezes
- 2) rhonchi
- 3) crackles
- 4) expiratory grunting
- 1) nasal flaring
2) substernal retractions
3) abdominal distention (seesaw breathing)

Pulmonological / CC BY-SA
- Primary assessment:
- 1) mature infant who requires mechanical ventilation and doesn’t improve
2) continued need for high oxygen concentrations
3) signs of respiratory distress (tachypnea, retractions)
- 1) mature infant who requires mechanical ventilation and doesn’t improve
- Diagnosis:
- CXR:
- 1) initially resembles IRDS then progresses to atelectasis, follow by cyst-like areas of hyperluency which increase in later stages
- ABG:
- acute alveolar hyperventilation with hypoxemia, develop hypercarbia later
- CXR:
- Management:
- A. oxygen therapy
- B. pulmonary hygiene
- C. mechanical ventilation for ventilatory failure
- D. ventilation and oxygenation should be maintained at the lowest possible level
- E. drug therapy: bronchodilators may be helpful
- F. monitor fluid balance
- G. surgical ligation of PDA for infants who are difficult to wean
- H. weaning from mechanical ventilation should be a slow, gradual process that involves higher concentrations of oxygen for prolonged periods of time after extubation. Infants may go home with oxygen therapy.
- I. supportive care to relieve symptoms of respiratory distress and heart failure
- J. maintain blood gas values: PaO2 55-70torr, PaCO2 45-60 torr, and pH 7.25-7.40
- K. minimize mean airway pressure
- L. extubation can be done at ventilator rates between 5-15 breaths/min
- M. avoid endotracheal CPAP, because of the increased airway resistance and work of breathing that can be created.
Common cold
- Path:
- Etiology:
- Transmission:
- Presentation:
- Complications:
- Diagnosis:
- Treatment:
- Prevention:
Croup (laryngotracheitis)
Cystic Fibrosis (CF)
- Path:
- Autosomal-recessive disease involving multiple organs, especially pancreas and lungs; most common lethal genetic disease in US; usually develop the obstructive disease (bronchiectasis), that leads to progressive respiratory failure and death;
- Presentation:
- with chronic sinusitis, nasal polyps, persistent cough, persistent and productive cough, infection and inflammation of the lungs eventually leads to bronchiectasis, pancreatic insufficiency leading to malabsorption and FTT, meconium ileus
- Diagnosis:
- Indications for Sweat Testing:
- Sweat Chloride Test:
- Treatment:
Osmosis / CC BY-SA
Cystic Fibrosis Symptoms
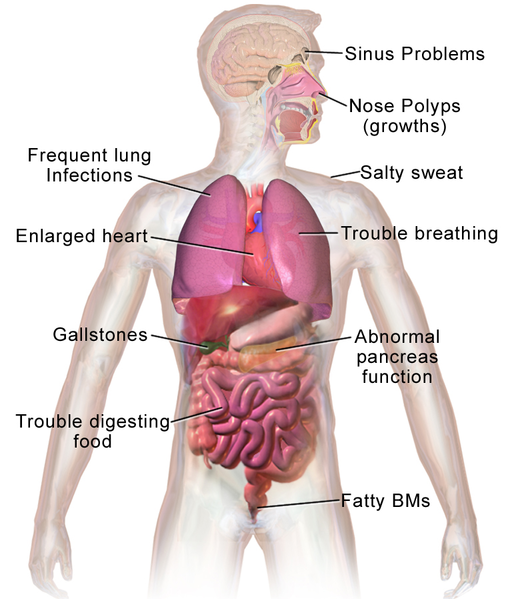
BruceBlaus. / CC BY
Epiglottitis
- Path:
- MC cause:
- Group A Streptococcus, S. aureus, H. influenzae type b (unimmunized)
- Radiograph:
- “thumb sign”
- Diagnosis:
- visualization when placing an endotracheal tube
- Management:

Med Chaos / CC0
Foreign body aspiration
IRDS (Infant Respiratory Distress Syndrome)
- Path:
- Primarily a disease of preterm infants
- deficiency of pulmonary surfactant in an immature lung
- noncompliant, stiff lungs that are structurally immature that contain an insufficient surfactant
- amount of pressure needed to open alveoli increase
- promotes hypoxemia, hypercarbia and then persistent pulmonary HTN
- Presentation:
- presents with prematurity (almost always), tachypnea, nasal flaring, expiratory grunting, intercostal, subxiphoid, and subcostal retractions, cyanosis, and diminished breath sounds
- Treatment:

Chest X-ray of a case of IRDS,
with fine granular opacities,
air bronchograms and bell-shaped thorax
Mikael Häggström, M.D. / CC0

Mikael Häggström, M.D. / CC0
Meconium Aspiration Syndrome (MAS)
- Path:
- Respiratory disease of term, postterm, and SGA newborns caused by inhalation of meconium or meconium-stained amniotic fluid into the lungs;
- Presentation:
- mild to severe respiratory distress, hyperexpansion of the chest, hyperinflated alveoli, and secondary atelectasis.
- Seen in 5% of newborns with meconium stained amniotic fluid
- Aspiration -.> airway obstruction -> respiratory distress
- Meconium effects on the lungs:
- Ball-valve effect
- Chemical irritation
- Predisposition for infection
- Inhibition of production + function of surfactant
- Often seen with primary pulmonary hypertension of the newborn (↑pulmonary vascular resistance)

Kinderradiologie Olgahospital Klinikum Stuttgart
/ CC BY-SA
- Diagnosis:
- X-ray: infiltrates, streaking, ↑A-P diameter, flattened diaphragm
- Management:
Newborn respiratory distress syndrome
- Feature:
- Premature babies
- Inadequate surfactant concentrations
- Preterm
- Respiratory Distress Syndrome (“Hyaline Membrane Disease”)
- Full-term
- Primary Pulmonary Hypertension of the Neonate (PPHN)
- Meconium Aspiration Pneumonia
- Preterm and full-term
- Transient Tachypnea of the Newborn
- Bacterial Sepsis (Group B Streptococcus)
- Premature babies
- Lab Evaluation:
- Chest X-Ray:
- Parenchymal pattern determination, ?pneumothorax, cardiac morphology
- Arterial Blood Gas:
- Acid-base disturbance, the extent of hypercapnia/hypoxia
- Complete Blood Count:
- H+H, white count, platelet count (?DIC)
- Blood Culture:
- Recovery of offending microbe
- Blood Glucose:
- Hypoglycemia, stress hyperglycemia
- Echocardiogram:
- Interrogation of murmur or PPHN, cardiomegaly, structural heart disease
- Chest X-Ray:
- Management:
Peritonsillar abscess
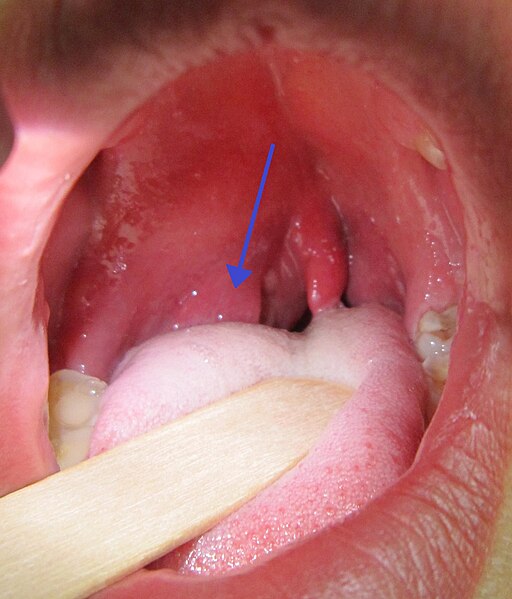
James Heilman,MD, CC BY-SA 3.0, via Wikimedia Commons
Peds Pneumonia
- About:
- An inflammation of lung parenchyma
- Viruses are the most common agents in infants
- Mycoplasma pneumoniae most common in children
- Bacterial PNA, bugs isolated from blood: strep pneumo, H. flu, Staph aureus in infants, debilitated pts, and adolescents with widely disseminated disease
- Predisposition to bacterial pna: aspiration, immunodeficiency, congenital anolamies (TE fistula, cleft palate) abnormal mucus clearance (CF, ciliary dysfunction ie Kartagener’s, bronchiectasis), CHF.
Bacterial Pneumoniae
- Microbiology by Age Group:
- ≤1 month:
- Group B Strep, E. coli, Gram (-) bacilli, S. pneumoniae
- 1-3 mos:
- Febrile
- RSV and other viruses
- Afebrile
- C. trachomatis, M. hominis, U. urealyticum, CMV, B. pertussis
- 3 months to 5 years:
- RSV + other viruses, S. pneumo, H. influenzae (type b, non-typeable),
- 5-18y:
- M. pneumoniae, S. pneumoniae, C. pneumoniae
- ≥18y:
- M. pneumoniae, S. pneumoniae, C. pneumoniae, H. influenzae (type b, non-typeable), influenza, adenovirus
- ≤1 month:
- Presentation:
- High fever, chills, wheeze, cough, dyspnea, consolidation (auscultatory findings)
- Physical Exam:
- Dullness to percussion à segmental infiltrates
- Complications:
- empyema & septicemia
- Sicklers are particularly susceptible to overwhelming pneumococcal infections.
- Diagnosis:
- CXR: lobar consolidation, round pneumonia + pleural effusion (10-30% of cases)
- Treatment:
- Typical Pneumonia:
- Neonates Group B or Listeria:
- 1-3 months peds:
- 3m- 5years peds:
- 5- 18 years peds:
- Empyema or pleural effusion:
- thoracentesis is diagnostic and therapeutic
- Surgical management:
- abscesses, pneumatocele, empyema
- For this patient, pneumonia can trigger a new asthma exacerbation
- Typical Pneumonia:
- Preschool kids (60 days – 5 years)
- Streptococcus pneumoniae and Haemophilus influenzae
- Treat with:
- amoxicillin
- 2nd – azithromycin or clarithromycin
- School-age kids (5-18)
- Mycoplasma pneumoniae and Chlamydia pneumoniae
- Treat with:
- azithromycin
Pneumococcal Pneumoniae
- Presentation:
- only signs may be fever + tachypnea.
- Treatment:
- Penicillin
Haemophilus influenza
- About:
- also lobar pna.
- Distinguished from pneumococcal pna by more indolent course and inadequate response to penicillin.
- Treatment:
- Abx include amox or amp PO but if PO inadequate may require IV amp.
- 20% of H. flu is resistant to amox/amp, use Augmentin or IV cephalosporin.
Staph Pneumoniae
- Presentation:
- most common in first year, usually unilateral, abscess, tissue destruction, overwhelming
septicemia.
- most common in first year, usually unilateral, abscess, tissue destruction, overwhelming
- 2 typical features:
- pneumatocele
- rapid progression.
- Empyema with thick purulent fluid is a hallmark.
- Treatment:
- chest tube for drainage
Mycoplasma Pneumoniae
- Presentation:
- #1 cause of adolescent pna (25-35%). Incubation period is 2-3 weeks.
- Sx of headache, malaise, fever, cough. WBC and diff usually normal, “cold agglutinins” may be + after 1st week of illness. CXR looks worse than the pt.
- Can be fulminant in SS dz pts.
- Assoc with bullous myringitis
- Treatment:
- Erythromycin.
Chlamydia trachomatis
- Presentation:
- contracted from birth thru infected vagina, usually presents at 1-2 months with low grade fever, machine gun or “staccato cough”. Increased eosinophils on differential.
- cxr will have diffuse interstitial infiltrate.
- 50% have proceeding conjunctivitis.
- Dx:
- by giemsa stain of conjunctival inclusion bodies.
- Treatment:
- Erythromycin.
Bordetella pertussis
- Presentation:
- 2000-4000 cases per year in US.
- Is an encapsulated gram-negative rod, infects ciliated epithelium of upper respiratory tract.
- Pertussis toxin increases adenylate cyclase, organism also synthesizes and exports adenylate cyclase.
- Association:
- apnea
- 3 stages of clinical dz:
- Catarrhal phase:
- lasts 2 weeks, coryza with increased mucus and secretions, sx similar to cold
- Paroxysmal phase:
- usually lasts 1-2 weeks but up to 4 weeks, consists of paroxysms of hacking cough with copious mucus followed by inspiratory ” whoop” air rushes past narrowed glottis.
- Convalescent phase:
- can last for months.
- Catarrhal phase:
- Dx:
- PCR
- culture on Bordet-gengou medium (high % of blood) ID by agglutination with specific antiserum or by fluorescent Ab staining.
- Treatment:
- Supportive: hydration, oxygen if needed
- Abx erythromycin, clarithromycin, azithromycin, TMP-SMX (halts spread, does NOT hasten recovery)
- close contacts – azithromycin
- Adults should get Tdap as a single booster dose
- Contraindications to giving pertussis vaccine:
- previous hx of serious reactions to vaccine (temp >105 or severe swelling at the injection site) seizure disorder or other significant neurological disorder
- Indication for admission:
- age <4-6 months, resp distress, toxic appearing, dehydration, vomiting if not taking PO’s, social factors, immunocompromised patients, esp sickler’s, CF patients
- Indic for d/c home:
- not hypoxic, good sats on room air, good PO intake, good UOP, negative bcx
Viral PNA
- MC cause:
- RSV, parainfluenza, influenza A & B
- Presentation:
- Cough, wheeze, stridor
- Less prominent fever
- Mucosal congestion, upper airway inflammation
- Diagnosis:
- CXR: diffuse infiltrates and hyperinflation
Primary ciliary dyskinesia
- Path:
- Presentation:
- mild respiratory distress, tachypnea, increased incidence of infections, chronic cough, symptoms increase over the course of the day
- constantly runny nose, year-round nasal congestion, rhinosinusitis
- defective Eustachian tube ciliary function leads to poor clearance, chronic otitis media, conductive hearing loss
- Association:
- Diagnosis:
- Management:
- Prognosis:
Reactive Airway Disease
Retropharyngeal abscess

Retropharygneal abcess
James Heilman, MD / CC BY-SA
Transient tachypnea of the newborn (TTN)
- Path:
- Presentation:
- Risk Factors:
- Diagnosis:
- Management:
Tuberculosis
Upper Respiratory Infections (Viral – URI)
- Management:
- OTC cough/cold medications NOT recommended, especially < 4 yo
- Buckwheat honey
- Pelargonium sidoides (geranium) extract (Umcka Coldcare)
- Nasal saline irrigation
- Vapor rub (> 2Yo)
- Zinc sulfate
- don’t use antibiotics
Reference
- Blausen.com staff (2014). “Cystic Fibrosis” Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.





