Table Of Contents
Abdominal Pain
- Common Causes of Acute Abdominal Pain in Neonates:
- Uncommon Causes of Acute Abdominal Pain in Neonates:
- Common Causes of Acute Abdominal Pain in Infants:
- Uncommon Causes of Acute Abdominal Pain in Infants:
- Common Causes of Acute Abdominal Pain in Preschoolers:
- Uncommon Causes of Acute Abdominal Pain in Preschoolers:
Acute Appendicitis
- Path:
- Most common condition requiring surgery:
- Presentation:
- Management:
Osmosis / CC BY-SA

Appedicitis on CT
James Heilman, MD / CC BY-SA
Celiac disease
- Path:
- An autoimmune disease caused by sensitivity to the protein gluten. Gluten is found in wheat, barley, and rye. If these grains are consumed by a child with celiac disease, an immune response is triggered and the damage is caused to the lining of the small intestine.
- Once the lining of the small intestines is damaged, nutrients can not be absorbed causing nutrient deficiencies. Some symptoms of celiac disease include: diarrhea, abdominal pain, abdominal distention, weight loss, fatigue
- About 3 percent of the US population has celiac disease.
- Diagnosis:
- Management:
- There is no cure for Celiac Disease.
- This condition can be managed by following a gluten-free diet. Children with celiac disease can lead to long, healthy lives.
- A few days after starting a gluten-free diet, children with celiac disease start gaining weight and symptoms (diarrhea, abdominal pain) resolve
- There is no cure for Celiac Disease.
- Meal Planning:
- Typical meals: B=eggs, oatmeal, smoothies (blueberries, mango, strawberries), L= almond banana sandwich or tuna with basmati rice and vegetables, S= cottage cheese (with fruits) or hummus w/cucumber and pretzels, D= orange chicken bowl or vegetarian tacos with vegetables and sweet potatoes.
- Grains/starches that are gluten-free: corn, quinoa, millet, rice, buckwheat, flax, lentils, potato, wild rice, soy, yucca, tapioca
- Foods that are naturally gluten-free: fruits, vegetables, beef, poultry, fish, nuts, eggs, most dairy
Cleft Lip and/or Cleft Palate
- Presentation:
- Facial malformations that occur during early (5-9wks) embryonic development
The lip and/or the palate do not fuse - May appear separately or together
- Facial malformations that occur during early (5-9wks) embryonic development
- Etiology:
- associated with chromosomal anomalies (Pierre Robin Syndrome), heart defects, ear malformations, skeletal deformities, genitourinary abnormality;
- Also associated with maternal smoking, prenatal infection, advanced maternal age, medications during early pregnancy (anticonvulsants, steroids)
Higher incidence in people of Asian, Native American, or Hispanic descent.
- Risk:
- Management:
- Post-surgical care:
Colic
- an infant between 2 weeks and 4 months of age who has crying episodes
- at least 3 times a week and longer than 3 hrs a day
- a child frequently outgrows the condition before the cause can be identified
Colitis
- Path:
- Ulcerative colitis is an inflammatory bowel disease (IBD) in which the lining of the large intestine (colon or bowel) and rectum becomes inflamed.
- Inflammation usually begins in the rectum and lower (sigmoid) intestine and spreads upward to the entire colon.
- Causes:
- diarrhea, or frequent emptying of the colon.
- As cells on the surface of the lining of the colon die and slough off, ulcers (open sores) form, causing pus, mucus, and bleeding.
- Presentation:
- Abdominal pain
- Bloody diarrhea
- Fatigue
- Weight loss
- Loss of appetite
- Rectal bleeding
- Loss of body fluids and nutrients
- Anemia caused by severe bleeding
Constipation
- Etiology:
- Presentation:
- Physical Exam:
- Imaging:
- Labs:
Encopresis
- About:
- Etiology:
- Treatment:
- Complications:
Esophagitis
Feeding Problems
Failure To Thrive
- Path:
- Epidemiology:
- Presentation:
- Prognosis:
- Cause:
- Organic disease cause:
Food allergies
- Path:
- food allergies result from an aberrant IgE mediated immune response
- -a reproducible immune mediated response to food
- -potentially life threatening
- -it is an IgE and Th2 mediated disease
- -results from a failure of oral tolerance
- -many influential factors including epithelial cell inflammation and environmental exposure
- MC cause:
- Tolerance:
- Self-tolerance:
- Central tolerance:
- Peripheral tolerance:
- if the self-reacting T cell gets out of the thymus and matures, they are removed by:
- 1. anergy = permanent functional unresponsiveness
- 2. suppression = active block in activation
- 3. deletion (apoptosis)
- Oral tolerance:
- you can eat the food whenever you want, how often you want, and as much or as little as you want
- Presentation:
- Immediate Hypersensitivity
- -most symptoms occur within 2 minutes
- -typically occur within 2 hrs
- -mediated by mast cell mediators
- Diagnosis:
- -Gold Standard: oral food challenge
- -most often made based on clinical history and confirmatory testing
- oral food challenge:
- ingest escalating amounts of a trigger food over several hours (dangerous)
- Food allergy testing:
- 1. skin prick testing (skin mast cell responsiveness)
- 2. serum IgE
-detection of food-specific IgE means that there is Ab capable of recognizing that food
- Serum IgE
- Dual Allergen Exposure Hypothesis:
- Treatment:
Gallbladder diseases
Gastroenteritis
- MC cause:
- Rotavirus and norovirus
- E.coli 0157 – leads to HUS
- Bloody stools – salmonella, shigella, campylobacter, enterocolitis, C. difficile
- Presentation:
- dehydration – abnormal respiratory pattern and skin turgor, prolonged capillary refill
- Diagnosis:
- stool studies only needed for diarrhea > 14 days or bloody
- Treatment:
- main – early oral rehydration solution (ORS)
- probiotics
- no anti-diarrheal
- resume a normal diet as soon as possible
Gastrointestinal bleeding
Gastroparesis
- Path:
- Associated:
- Cause:
Gastroesophageal Reflux (GERD)
Hirschsprung Disease
- Path:
- Presentation:
- Associated:
- Diagnosis:
- – barium enema: narrowed distal
colon with proximal dilation - – x-ray: distended bowel loops with a paucity of air in the rectum
- – anorectal manometry: detects failure of the internal sphincter to relax after distention of the rectal lumen
- – rectal biopsy: absence of the myenteric
(Auerbach) plexus and submucosal (Meissner) plexus
- – barium enema: narrowed distal
Hypertrophic Pyloric Stenosis
- Path:
- Presentation:
- Evaluation:
- Physical Exam:
- Labs:
- Management:
- Provide fluids via IV fluids and electrolytes
NG tube for stomach decompression - The nasogastric tube provides decompression and decreases vomiting.
- Severely dehydrated children will have a 5 day course of IV fluids and electrolyte replacement, and infusions of PRBC.
- Pyloromyotomy – Incision of pyloric muscle to release obstruction (definitive treatment) Prognosis is good with few complications.
- Provide fluids via IV fluids and electrolytes
Inflammatory bowel disease
Crohn’s Disease
- Presentation:
- Features:
Osmosis / CC BY-SA
- Diagnosis:
- +/- ASCA
- Barium: String Sign
- colonoscopy: Skip Lesions, Cobblestone Appearance
Ulcerative Colitis
- Path:
- Presentation:
- Diagnosis:
- Management:
- Complications:
Intestinal Atresia
- Types:
- 1) Duodenal: “Double-bubble”
- 2) jejunal/ilieal: “Apple-core”
Duodenal Atresia
Intractable Vomiting
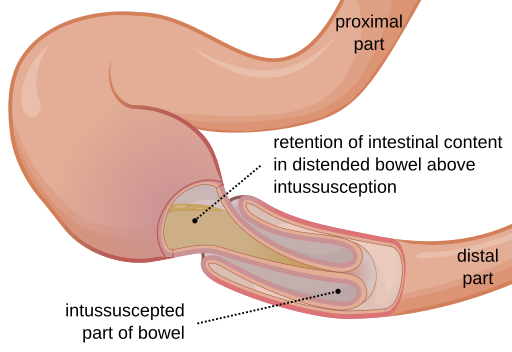
Intussusception
- Path:
- Epidemiology:
- Presentation:
- Physical Exam:
- Risk Factor:
- Diagnosis:
- Labs:
- Priority interventions:
Irritable bowel syndrome
- Presentation:
- Recurring Belly pain
- Continuous Pain for more than 3 months is long-term (chronic).
- Diarrhea or constipation
- Upset stomach (nausea)
- Dizziness
- Loss of appetite
- Swelling (bloating) and gas
- Cramping
- Immediate bowel movement
- incomplete emptying
- Mucus in the stool
- Cause:
- Problems with how food moves through their digestive system
- Extreme sensitivity of the inside of their bowel to stretching and motion
- Stress
- Too much bacteria growing in their bowel
- Risks:
- Family history
- Teens > younger children
- Affects boys and girls equally
Osmosis / CC BY-SA
- Diagnosis:
- Blood tests – anemia, an infection, or an illness caused by inflammation or irritation.
- Urine analysis and culture – help check for urinary tract infections.
- Stool sample – checks for bacteria and parasites that may cause diarrhea.
- Stool samples for occult blood – If blood is found, there may be inflammation in the GI (gastrointestinal) tract.
- Lactose breath hydrogen test – see if child can’t digest lactose (is lactose intolerant).
- Abdominal X-ray
- Abdominal ultrasound
- EGD (esophagogastroduodenoscopy) or upper endoscopy)
- Colonoscopy
- Management:
- Lactose intolerant – limit lactose.
- Use lactase/Lactaid
- High fiber for children who have constipation.
- Add good bacteria (probiotics) regulated by the FDA.
- Stress management
Intestinal pseudo-obstruction
Liver disease
Malabsorption
Malrotation with volvulus
Meckel Diverticulum
- Presentation:
- Rule of 2’s:
- Diagnosis:
- Treatment:
- Complications:
Motility disorders
Necrotizing enterocolitis
- Presentation:
- MC location:
- Risk Factors:
- Acute Complications:
- Chronic Complications:
- Diagnosis:
- Management:
Nutrition Issues
Pancreatic diseases
- 1) Annular Pancreas: Ventral bud encircling and strangling 2nd portion of the duodenum. Non-bilious vomiting
- 2) Pancreatic divisum: Lack of ventral/dorsal bud fusion. Chronic pancreatitis.
Parasitic Infections
Peptic ulcers
Polyps
Obesity
Short gut (bowel) syndrome
- Path:
- Associated:
- Presentation:
- Complications:
- – Bacterial overgrowth in the small intestine
- – Degeneration of the nervous system caused by a lack of vitamin B12 (combined systems disease)
- – Excess acid in the blood (metabolic acidosis due to diarrhea)
- – Gallstones
- – Kidney stones
- – Malnutrition
- – Too much growth of bacteria
- – Weakened bones (osteomalacia)
- – Weight loss
- – Bacterial overgrowth in the small intestine
- Diagnosis:
- Treatment:
Tracheoesophageal Fistula
- Path:
- abnormal connection between the esophagus and trachea
- infants with EA cannot clear their secretions. leads to persistent drooling and aspiration or regurgitation of food after attempted feedings
- infants with this anomaly strain, cough, or cry, air enters the stomach through the fistula.
- the stomach and small intestine become dilated, elevating the diaphragm and making respiration more difficult
- The reflux of food and gastric secretions may also occur up the esophagus and through the fistula into the tracheobronchial tree; this reflux can contribute to pneumonia and atelectasis. Therefore, pneumonia and respiratory distress are common complications.
- Presentation:
- Drooling/vomiting with the first meal
- 1. infant with EA has maternal polyhydramnios
- 2. prenatal US can reveal the stomach’s gas absence.
- 3. neonatal period, excess salivation with large amounts of white frothy bubbles in the mouth and nose. bubbles recur despite repeated suctioning.
- 4.signs of respiratory distress symptoms and recurrent pneumonia
- 5.Coughing, choking and cyanosis during feeding
- Most TEF present almost immediately after birth.
- Food cannot get to the stomach, resulting in immediate emesis and rapid dehydration.
- Gastric contents may enter the lungs, resulting in respiratory distress.
- MC Subtypes:
- 1.Esophageal atresia with distal tracheoesophageal fistula
- 2.Isolated esophageal atresia without a tracheoesophageal fistula
- 3.H type esophageal fistula without atresia
- 4.Isolated esophageal atresia without tracheoesophageal fistula (proximal esophagus feeds into trachea no path to the stomach)
- 5.Esophageal atresia with proximal and distal communications
- 1.Esophageal atresia with distal tracheoesophageal fistula
- Association:
“File:Tracheoesophageal Fistula Types.svg” by Jmarchn is licensed under CC BY-SA 3.0
- Diagnosis:
- screening tool Prenatal US reveal polyhydramnios, the absence of gas in the stomach, a distended esophageal pouch, and in-utero growth retardation.
- Plain x-ray – exclude complications such as aspiration pneumonia and to have more clues to confirm the diagnosis
- Nasogastric tube insertion – inserted to confirm the diagnosis of esophageal atresia. as the nasogastric tube will coil in the mediastinum and one would visualize the radiopaque line of the catheter.
- Multidetector-row computed tomography scans – used to confirm the diagnosis of a tracheoesophageal fistula without the use of a contrast medium.
- Treatment:
- 1. Echocardiography – performed prior to surgery to rule out a right-sided aortic arch.
- 2. Surgical repair – performed under general anesthesia with endotracheal intubation.
- 3. Surgical repair – delayed in neonates with very low birth weight or aspiration pneumonia. All other infants should be operated within the first days of life.
- 4. Surgery involves Primary ligation of the fistula and anastomosis of the esophageal segments