Gram Indeterminate Bacteria section provides High Yield Information needed for USMLE, COMLEX, Medical School, Residency, and as a practicing Physician.
Table Of Contents

LadyofHats / Public domain
Borrelia Burgdorferi
- Features:
- Wright’s stain and Giemsa stain
- Spiral shaped- spirochete
- Seen in Northeastern US
- Causes:
- Lyme disease
- History of hiking or recent camping
- Transmission: Ixodes tick: humans incidental host
- Clinical presentation: 3 stages
- – Stage 1: characteristic rash: Bull’s eye/erythema chronicum migrans
- non-painful or pruritic, one month after tick rash *HALLMARK* of Lyme disease
- – Stage 2: heart block due to myocarditis and bilateral facial nerve palsy/Bell’s palsy
- – Stage 3: migratory polyarthritis – commonly large joints, Encephalopathy- memory difficulty, cognitive slowing, lymphocytic meningitis
- – Stage 1: characteristic rash: Bull’s eye/erythema chronicum migrans
- Treatment:
- – Doxycycline- for early treatment
- – Ceftriaxone- for later stages of Lyme disease

Borrelia Burgdorferi
Photo Credit:Content Providers(s): CDC / Public domain

Bull’s Eye Rash
Photo Credit: James GathanyContent Providers(s): CDC/ James Gathany / Public domain
Leptospira Interrogans
- Features:
- Spirochete- question mark shaped
- Causes:
- Leptospirosis
- Reservoir: rodents and dogs excreted in urine
- Transmission: humans swimming in contaminated water
- Clinical manifestations:
- Early
- – Flu like symptoms: fever and intense headaches
- – Conjunctival suffusion
- Systemic/Leptospirosis/Weils disease
- – hematogenous spread–> kidney and liver
- – kidney: fever, high creatinine and azotemia–> kidney dysfunction
- – liver: liver dysfunction and jaundice
- Early
- Treatment:
- Doxycycline
- Ceftriaxone

Leptospira Interrogans
Obtained from the CDC Public Health Image Library.Image credit: CDC/NCID/HIP/Janice Carr (PHIL #1220). / Public domain

Cerevisae / CC BY-SA
Treponema Pallidum
- Features:
- Spirochete – spiral-shaped
- Causes: syphilis
- Transmission: Sexually transmitted
- Visualization via dark field microscopy
- Blood test- most commonly used for diagnosis
- Screening:
- – VDRL — non-specific
- – FTA-Ab test- confirmation test
- Clinical manifestations:
- Early Stages-Occurs first year of infection
- – Primary: Painless genital chancre, weeks after inoculation. ischemia–> nerve damage and necrosis. heals in 3-6 weeks. if not treated, will progress to a secondary stage
- – Secondary: systemic disease- maculopapular rash on palms and soles weeks to months after infection. condyloma lata- flat-topped lesions on mucous membranes
- Late stages:
- Tertiary: Gummas- soft growths with a firm necrotic center- seen systemically, Aortitis: most commonly affecting ascending thoracic aortic -> aneurysm tree barking, Tabes dorsalis – demyelination of posterior column, Ocular effects- neuronal damage- Argyll
- Robertson pupils- reacts to accommodation but not to light
- Congenital syphilis
- – Saber shins- anterior bowing of the tibia
- – Saddle shaped nose
- – Hutchinson’s teeth
- – Congenital deafness
- – Hepatomegaly, rhinitis, rash
- Early Stages-Occurs first year of infection
- Treatment:
- – Penicillin
- – Allergy to penicillin- Tetracycline
- Jarisch-Herxheimer reaction:
- – dying spirochetes giving out LPS–> increase in cytokines
- – Fever, chills, and headache within hours of treatment

Treponema Pallidum
Photo credit:Content providers(s): CDC / Dr. David Cox / Public domain

Primary: Genital Chancre
The original uploader was Pygmalion at German Wikipedia. / CC BY-SA
Secondary Syphilis – maculopapular rash on palms and soles
Centers for Disease Control and Prevention (CDC) / Public domain

Tertiary Syphilis – Gumma on nose
CDC/ J. Pledger / Public domain
Chlamydia Trachomatis
- Features:
- Gram indeterminate- lack gram stain
- obligate intracellular bacteria
- lack muramic acid in cell wall
- Elementary bodies: stage 1, infectious form, bacteria outside cell, no multiplication
- Reticular body: stage 2, dividing by binary fission, active form of bacteria that multiplies
- Inclusion bodies seen under microscope
- Diagnosis: NAAT
- 3 groups of chlamydia trachomatis:
- A-C
- D-K = STI most commonly reported in US
- L1-L3
- 3 groups of chlamydia trachomatis:
- Symptoms:
- watery discharge, can worsen to become PID, neonatal conjunctivitis, neonatal pneumonia 1-2 weeks after birth
- L1-L3–> lymphogranuloma veneremum/LGV
- STI less common than D-K
- infection of lymphatics especially inguinal
- symptoms: painless genital ulcer, weeks to months later- tender lymphadenopathy wit draining lymph nodes
- A-C–> associated with trachoma- leading cause of blindness worldwide.
- Complications of infection
- – PID (like gonorrhea)
- – Reactive arthritis/Reiter’s syndrome “Can’t see, Can’t pee, Can’t climb a tree”
- Treatment:
- – Macrolide: Azithromycin
- – Topical Azithromycin for neonatal conjunctivitis
- – Tetracycline: Doxycycline- second line
- – Co-infection with N gonorrhea: Azithromycin and Ceftriaxone
Chlamydia Trachomatis
User Marcus007 on de.wikipedia / Public domain
Chlamydia Pneumonia
- Features:
- Gram indeterminate- lack gram stain
- obligate intracellular bacteria
- lack muramic acid in cell wall
- Path:
- Elementary bodies: stage 1, infectious form, bacteria outside cell, no multiplication
- Reticular body: stage 2, dividing by binary fission, active form of bacteria that multiplies
- Causes atypical/walking pneumonia like mycoplasma and legionella
- More common in:
- elderly
- Treatment:
- Tetracycline: Doxycylcine DOC
- Macrolide: Azythromycin 2nd line

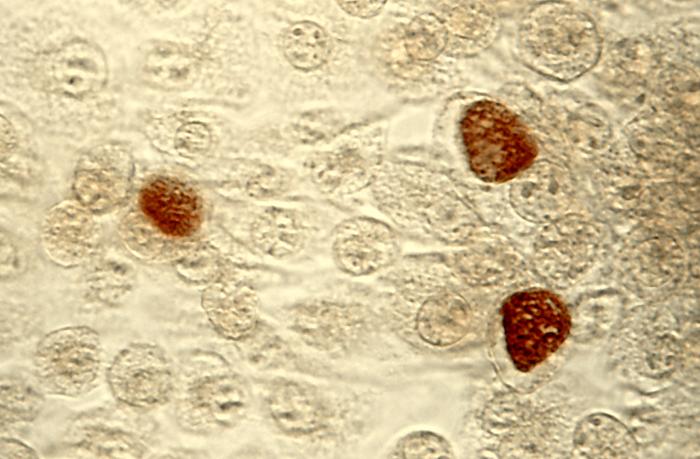
Micrograph of Chlamydia pneumoniae in an epithelial cell in acute bronchitis:
1 – infected epitheliocyte,
2 – uninfected epitheliocytes,
3 – chlamydial inclusion bodies in cell,
4 – cell nuclei
Eutensist / Public domain
Chlamydia Psittaci
- Features:
- Gram indeterminate- lack gram stain
- obligate intracellular bacteria
- lack muramic acid in cell wall
- Path:
- Elementary bodies: stage 1, infectious form, bacteria outside cell, no multiplication
- Reticular body: stage 2, dividing by binary fission, active form of bacteria that multiplies
- Causes pneumonia
- Transmission:
- birds often parrots

Chlamydia Psittaci
Photo Credit:Content Providers(s): CDC/Dr. Vester Lewis / Public domain
Coxiella Burnetii
- Features:
- Gram negative
- Obligate intracellular
- Spore former- survive in GIT of animals and soil
- Transmission:
- aerosol
- Major Reservoir:
- Farm animals
- Farmer infected by farm animal, Veterinarian who did surgery on farm animal
- Causes:
- – Causes Q fever
- – Pneumonia
- – Headache
- – Fever
- – Hepatitis
- Treatment:
- – Self limiting- no antibiotics needed goes away within 2 weeks
- Prevention:
- – Pasteurizing milk
- – Acellular vaccination – those who work closely with animals
 “Coxiella burnetii Bacteria” by NIAID is licensed under CC BY 2.0
“Coxiella burnetii Bacteria” by NIAID is licensed under CC BY 2.0

A: Normal Lung
B: Q fever Pneumonia
See page for author / Public domain
Gardnerella Vaginalis

Gardnerella Vaginalis
Dr. F.C. Turner / Public domain

Bacterial Vaginosis – Clue Cells
Per Grinsted / Medicinsk Webdesign / CC BY-SA
Mycoplasma Pneumoniae
Rickettsia
- Features:
- – white Gram indeterminate
- – gram neg but don’t gram stain well aka Pleomorphic
- – Obligate intracellular
- – Colonize Endothelial Cells and cause endothelial hyperplasia
- – NAD+ water bottle held by CoAch – Unable to produce NAD+ and CoA, so both are important for bacterial growth and replication
- – Coccobacillary Shape that are weakly gram negative
- – Weil Felix agglutination test for rickettsia infections
- – Prodromal Headache and fever in early rickettsia, along with VASCULITIS. Inflammation and destruction
- – Vasculitis
- – Rash
- Treatment:
- – Doxcycline:
- – Chloramphenicol if pregnant
- – Supportive care with vascular collapse

Rickettsia
CDC / Public domain
Rickettsia Prowazekii
- Features:
- Coccobacillary shape
- Obligate intracellular
- Poor gram staining- weakly gram negative
- Vector: louse
- Transmission: louse bites, excretes and patient scratches
- Clinical manifestation:
- Early: headache, fever, vasculitis
- Rash: trunk–> extremities SPARES Hands and feet
- myalgia, arthralgia, pneumonia, encephalitis, coma
- At risk: close contact
- Diagnosis: Weil Felix test
- Treatment:
- Doxycycline
Ricketsia Rickettsii
- Features:
- Coccobacilliary shape
- Obligate intracellular
- Poor gram staining- weak gram negative
- Transmission:
- tick (dermacentor) direct bite
- Clinical presentation:
- – progression of rash: rash not immediate 2-14 days
- – rash starts on hands and feet and progress towards trunk
- – headache, fever and myalgia
- Treatment: Doxycycline
Bacteria Gram Indeterminate Quiz 1
0 votes, 0 avg
1Bacteria Gram Indeterminate Quiz 2
0 votes, 0 avg
0