The EKG-Electrocardiogram section provides High Yield Information that is needed for the USMLE and COMLEX exams, Medical School, Residency, and as a practicing Physicians.
Table Of Contents
EKG Interpretation
Steps to read the EKG
- Determine Rate (300/#big boxes ~ 60-100bpm)
- Determine Rhythm (P:QRS ratio)
- P waves
- PR interval (0.12-0.2)
- QRS Complex (0.06-0.12)
P wave: atrial depolarization (atrial contraction/systole)
(0.7-0.12)
QRS complex: ventricular depolarization (contraction/systole) and hidden atrial repolarization (diastole)
(0.05-0.10)
T wave: ventricular repolarization and relaxation
PR interval: line from the end of the p wave to the onset of the QRS complex
AV node delay
(0.12-0.2 –> 3-5mm)
Types of Rhythm
- Normal Sinus Rhythm
- Sinus Bradycardia
- Sinus Tachycardia
Atrial- Premature Atrial Contractions
- Atrial Flutter
- Atrial Fibrillation
- Multifocal Atrial Tachycardia
Ventricular- Premature Ventricular Contractions
- Accelerated Idioventricular Rhythm
- Ventricular Fibrillation
- Monomorphic Ventricular Tachycardia
- Polymorphic Ventricular Tachycardia
Junctional- Junctional Rhythm
- Junctional Tachycardia
- Premature Junctional Contraction
- Supraventricular Tachycardia
Pacemaker- Atrial pacing rhythm
- Wandering Atrial Pacemaker
- Ventricular pacing rhythm
- Dual A/V pacing rhythm
- Biventricle pacing rhythm
Asystole
- Def:
Causes:
Presentation:- Patient will not have a pulse or blood pressure, a code blue!
Glenlarson / Public domain
Atrial Fibrillation
- Presentation:
- 1) ASx
- 2) SOB
- 3) Chest Pain
- 4) palpitations
- 5) irregularly irregular pulse
EKG:- no P waves, with variable and irregular QRS response
Acute: PIRATES- 1) Pulmonary disease
- 2) Ischemia
- 3) Rheumatic heart disease
- 4) Anemia/Atrial myxoma
- 5) Thyrotoxicosis
- 6) Ethanol
- 7) Sepsis
Chronic:- 1) HTN
- 2) CHF
Management:- If unstable
– synchornized electrical cardioversion starting at 100J - If stable
– control rate w/ diltiazem or B-blockers and anticoagulate if duration is >48hrs
– Elective cardioversion may be performed if <48hrs; or need to anticoagulate and perform TEE prior to conversion - Do not give nodal blockers if there is evidence of WPW syndrome on EKG
- If unstable
- Calculators:
Osmosis / CC BY-SA
- Calculate CHAD2 Score
1) Anticoag if > 48hrs
2) rate control (B-blockers, CCB, digoxin)
3) Rhythm control (cardioversion, amiodarone) - initiate cardioversion only if new onset <48hrs or if TEE shows no left atrial clot, or after 306wks of warfarin tx
CHADS2 Score:- C-Congestive heart failure = 1 point
- H-Hypertension = 1 point
- A-Age ≥75 years = 1 point
- D-Diabetes = 1 point
- S-Stroke/TIA = 2 points
- 0 Low None
- 1 Intermediate/moderate
- 2 or > Intermediate or High
CHA2D2-VASc Score:- C: CHF/LV dysfunction 1 point
- H: HTN 1 point
- A: Age ≥75 years 2 points
- D: Diabetes 1 point
- S: Stroke/TIA 2 points
- V: Vascular disease 1 point (prior MI, PAD, or aortic plaque)
- A: Age 65-74 years 1 point
- S: Sex (female) 1 point
- CHA2DS2-VASc score of:
- 0: No risk
- 1: Intermediate risk
- ≥2: High risk
- 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation
Management using CHADS2/CHA2DS2-Vasc:- CHADS2 should be used as the initial method for stroke stratification in pts with Afib!! If CHADS2 score of 0-1, perform CHA2DS2-VASc!! If CHADS2 score 2 or greater, prescribe warfarin (INR 2-3)
- CHA2DS2-VASc score = 0 – ASA or NO antithrombotic therapy (no therapy preferred)
- CHA2DS2-VASc score = 1 – warfarin or ASA (warfarin preferred)
- CHA2DS2 – VASc score = 2 or greater = warfarin
Atrial Flutter
- Presentation:
- 1) Asymptomatic
- 2) palpitations
- 3) Syncope
- 4) lightheadedness
EKG:- regular rhythm;
- “sawtooth” appearance of P waves;
- rate 240-320bpm w/ varying degrees of blockade
Management:- If unstable
– synchronized electrical cardioversion starting at 100J - If stable
– control rate w/ diltiazem or B-blockers and anticoagulate if duration is >48hrs
– Elective cardioversion may be performed if <48hrs; or need to anticoagulate and perform TEE prior to conversion - Do not give nodal blockers if there is evidence of WPW syndrome on EKG
- anticoagulation and rate control, cardiovert like Afib
- If unstable
Atrial Ventricular Block
First degree AV block
- Causes:
- 1) none
- 2) increased vagal tone
- 3) B-blocker/CCB use
EKG:- PR interval > 200 msec
Second degree AV block (Mobitz I/Wenckebach)
- EKG:
- progressive PR lengthening until a dropped beat occurs;
- PR interval then resets
Causes:- 1) drug effects (digoxin, B-blockers, CCBs)
- 2) increased vagal tone
- 3) sinoatrial conduction disease
- 4) R coronary ischemia or infarction
Treatments:- 1) stop offending drug
- 2) Atropine
- 3) pacemaker placement
Second degree AV block (Mobitz II)
- EKG:
- unexpected dropped beat(s) w/o a change in PR interval
Presentation:- 1) occasionally syncope
- 2) frequent progression to third-degree AV block
Causes:- 1) fibrotic disease of conduction system
2) acute/subacute/prior MI
- 1) fibrotic disease of conduction system
Treatments:- pacemaker placement
Third-degree AV block (complete heart block)
- EKG:
- no relationship btw P and QRS waves
Presentation:- 1) syncope
- 2) dizziness
- 3) acute heart failure
- 4) hypotension
- 5) cannon A waves
Treatments:- pacemaker pacemaker

MoodyGroove at English Wikipedia / Public domain
AVNRT
- EKG:
- Rate 150-250bpm
- P wave buried in QRS or shortly after
Presentation:- palpitations
- SOB
- angina
- syncope
- lightheadedness
Management:- carotid massage; Valsalva; adenosine can stop the arrhythmia
- cardiovert if hemodynamically unstable
AVRT
- EKG:
- the retrograde P wave is often seen after a normal QRS
Presentation:- palpitations
- SOB
- angina
- syncope
- lightheadedness
Management:- carotid massage, Valsalva, or adenosine can stop the arrhythmia.
- cardiovert if hemodynamically unstable
Brugada syndrome
Multifocal atrial tachycardia
- EKG:
- three or more unique P-wave morphologies and rate >100bpm
Causes:- multiple atrial pacemakers
- reentrant pathways
- COPD
- hypoxemia
Management:- 1) treat the underlying disorder
- 2) verapamil or B-blockers for rate control and suppression of atrial pacemakers (not very effective)
Paroxysmal atrial tachycardia
- EKG:
- rate >100 bpm;
- P wave w/ an unusual axis before each normal QRS
Presentation:- palpitations
- SOB
- angina
- syncope
- lightheadedness
Management:- adenosine to unmask underlying atrial activity
Premature ventricular contraction (PVC)
- EKG:
- early, wide QRS no preceded by a P wave. PVCs are usually followed by a compensatory pause
Causes:- ectopic beats arise from ventricular foci; hypoxia; electrolyte abnormalities; hyperthyroidism
Management:- treat underlying cause;
- if symptomatic give B-blockers or occasionally other antiarrhythmics
Pulseless electrical activity
- Causes:
- 5Hs and 5Ts
- Hypovolemia
- Hypoxia
- Hydrogen ion: acidosis
- Hyper/HypoK other metabolic
- Hypothermia
- Tablets: Drug OD, ingestion
- Tamponade: cardiac
- Tension pneumothorax
- Thrombosis: coronary
- Thrombosis: PE
Management:- epinephrine or vasopressin; simultaneously search for the underlying cause and provide empiric tx
- bradycardic PEA only – Give atropine

Masur / Public domain
Sick sinus syndrome (tachycardia-bradycardia syndrome)
- Presentation:
- syncope
- palpitations
- dyspnea
- chest pain
- TIA
- stroke
Management:- pacemaker placement
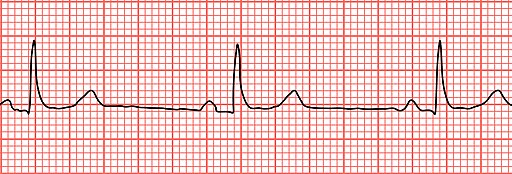
Sinus Bradycardia
- Presentation:
- 1) Asymptomatic
- 2) lightheadedness
- 3) syncope
- 4) chest pain
- 5) hypotension
Management:- If symptomatic
- – give atropine (to increase HR) and consider dopamine, epinephrine, and glucagon
- If Mobitz II or third-degree heart block is present
- – place transcutaneous pacemaker pads, and have atropine at the bedside
- If hemodynamically unstable pts
- – A temp transvenous pacemaker may be required
- If symptomatic
Sinus Tachycardia
- Presentation:
- 1) palpitations
- 2) shortness of breath
Conditions Suggest:- 1) fear
- 2) pain
- 3) exercise
- 4) hyperthyroidism
- 5) volume contraction
- 6) infection
- 7) pulmonary embolism
 “File:Sinus Tachycardia Unlabeled.jpg”
“File:Sinus Tachycardia Unlabeled.jpg”
by Andrewmeyerson is licensed under CC BY-SA 3.0
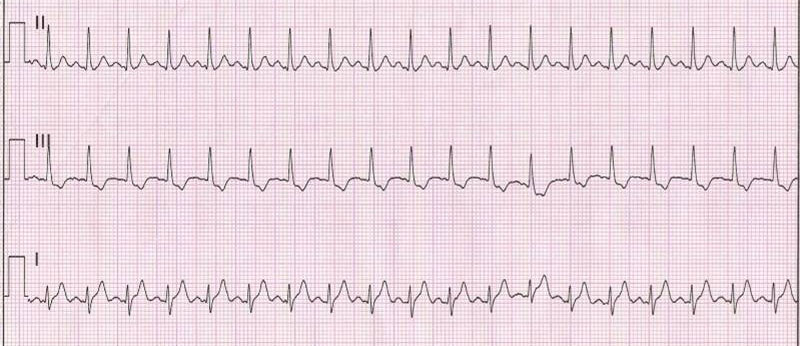
Supraventricular Tachycardia
- Management:
- If unstable
- – perform synchronized electrical cardioversion
- If stable
- – control rate w/ vagal maneuvers (Valsalva maneuver, carotid sinus massage, or cold stimulus)
- If resistant to maneuvers
- – give up three doses of adenosine followed by other AV nodal blocking agents (CCBs or B-blockers)
- If unstable
SVT_Lead_II.JPG: Displacedderivative work:
James Heilman, MD / Public domain
Torsades de pointes
- Causes:
- associated with
- long QT syndrome
- proarrhythmic response to meds
- hypokalemia
- congenital deafness
Management:- Correct hypokalemia,
- withdraw offending agent,
- give Mag initially and
- cardiovert if unstable

Displaced / Public domain
Ventricular Fibrillation
- Management:
- immediate electrical cardioversion and ACLS protocol
- unsynchronized shock w/ 360J–>360-J shock–>epinephrine–>360-J shock–>amiodarone or lidocaine–>360-J shock–>epinephrine
- Vasopressin can be given in place of the 1st or 2nd dose of epinephrine
- – amiodarone, lidocaine, procainamide, or sotalol may be used for stable Vtach
Osmosis / CC BY-SA
Glenlarson / Public domain
Ventricular Tachycardia
- Management:
- Cardioversion
- unsynchronized shock w/ 360J–>360-J shock–>epinephrine–>360-J shock–>amiodarone or lidocaine–>360-J shock–>epinephrine
- Vasopressin can be given in place of the 1st or 2nd dose of epinephrine
- – amiodarone, lidocaine, procainamide, or sotalol may be used for stable Vtach
Osmosis / CC BY-SA
Glenlarson / Public domain
Wolff-Parkinson-White Syndrome
- Causes:
Presentation:
ECG:
Management:
Cause of death:
EKG
| Interval | Normal | Long |
| PR | 120-200msec | |
| QRS | <100msec | |
| QT | QTc>440msec |
| LBBB | QRS>120msec; no R wave in V1; tall R waves in I, V5, and V6; W pattern of QRS in V1 and V2 and M pattern for QRS in V3-V6 |
| RBBB | QRS >120ssec; RSR’ complex; qR or R morphology with a wide R wave in V1; QRS pattern with a wide S wave in I, V5, V6; M pattern of QRS in V1 and V2; and W pattern of QRS in V3-V6 |
| Ischemia | inverted T waves; poor R wave progression in precordial leads; ST-segment changes (elevation/depression) |
| Transmural Infarct | significant Q waves (>40msec or more than 1/3 of the QRS amplitude). ST elevation; T wave inversion; presence of possible impending infarction based on plaque instability |
| L Atrial Hypertrophy | P wave width in II >120msec or if terminal negative deflection in V1 is >1mm in amplitude and >40msec in duration |
| R Atrial Hypertrophy | P wave amplitude in II <2.5mm |
| LVH | Amplitude of R in aVL + S in V3>28mm in men and 20mm in women OR S in V1 + R in V5 or V6>35mm |
| RVH | R axis deviation and R wave in V1>7mm |
EKG Practice
Clinical Signs
| Suggested Conditions | |
| JVD | 1) R heart failure 2) pulmonary hypertension 3) volume overload 4) tricuspid regurg 5) pericardial disease 6) Hepatojugular reflux: fluid overload; impaired RV compliance |
| Kussmaul’s sign | Def: Increased JVP w/ inspiration 1) RV infarction 2) Postop cardiac tamponade 3) tricuspid regurgitation 4) constrictive pericarditis |
| S3 Gallop | Ventricle Gallop 1) dilated cardiomyopathy (floppy ventricle) 2) mitral valve disease 3) normal in younger pts and in high-output states (pregnancy) |
| S4 Gallop | Atrial Gallop 1) HTN 2) diastolic dysfunction (stiff ventricle) 3) aortic stenosis 4) normal in younger pts and athletes |
| Respiratory crackles | pulmonary edema/effusion |
| Peripheral edema | 1) RHF 2) biventricular failure 3) peripheral venous disease 4) constrictive pericarditis 5) tricuspid regurgitation 6) hepatic disease 7) lymphedema 8) nephrotic syndrome 9) hypoalbuminemia 10) drugs |
| Pulsus alternans | Def: alternating weak and strong pulses 1) cardiac tamponade 2) impaired LV systolic fxn 3) poor prognosis |
| Pulsus paradoxus | Def: decreased SBP w/ inspiration 1) pericardial tamponade 2) asthma and COPD 3) tension pneumothorax 4) foreign body in the airway |
| Pulsus parvus et tardus | Def: weak and delayed pulse aortic stenosis |