Dermatology Treatments for many of the common diseases that are in the USMLE Steps 1, 2, 3, COMLEX Level 1,2,3, and Residency. High Yield resources for medical students and resident physicians.
Atopic dermatitis (eczema)
- Presentation:
- -usually occurs in children; onset after age 30 is rare; may be pruritic, exudative, or lichenified and located in the face, neck, trunk, wrists, hands, antecubital fossa, popliteal folds; symptoms include: itching, rough red plaques
- Pathophysiology:
- increased T cell activation; abnormal cell-mediated immunity; overproduction of IgE
- Physical Exam:
- -“itch-scratch cycle”; acute-erythematous papules/plaques with poorly defined border; chronic lichenification and painful fissures; excorations are common; Dennie Morgan sign
- Dx:
- -increase in serum IgE levels; RAST allergy testing; viral cultures to rule out other infections
- Management:
- avoiding triggers
- topical corticosteroids
- nonsteroidal immunomodulators (tacrolimus)
- leukotriene inhibitors
- acute lesions may require wet dressings
- chronic – necessary to maintain daily hydration with unscented bath soaps and emollients
 “Eczema versus Fingerprints 2009” by mazpho.to is licensed under CC BY-SA 2.0
“Eczema versus Fingerprints 2009” by mazpho.to is licensed under CC BY-SA 2.0
Condyloma Acuminatum
- Presentation:
- -genital warts (HPV6&11); high risk = HPV 16, 18, 31, 33, and 45; low risk = HPV 1, 6, and 11
- -90% of HPV infections are cleared from the body within 2 years of infection
- Transmission:
- via skin-to-skin contact
- 90% of people who contract HPV do not develop warts but are still contagious
- presence of visible warts may be an indication of increased infectivity
- vertical transmission at birth
- sexual transmission = the most common viral STI
- non-sexual transmission = cutaneous transmission to hands
- sharing of clothing; incubation period = 2-3 months
- Latency:
- possibility for virus to become latent
- latent patients are still able to transmit the disease
- 1/3 of patients with warts will experience recurrence
- Physical Exam:
- -may our singly, most commonly found in clusters; papules or plaques with cleft surface; any part of oral, anal, or genital region; most common on surface, can be found internally; can be soft or firm, in a variety of colors and may bleed; possible itching, discomfort, pain
- Dx:
- clinical dx
- pap smear
- biopsy to confirm
- microscopic: enlargement of dermal papillae; parakeratosis; nuclear enlargement with perinuclear clearing; papillomatosis koilocytes
Contact dermatitis
- Presentation:
- -most commonly caused by contact with poison oak/ivy, topical antimicrobials
- -occupational exposure is an important cause
- -tiny vesicle formation and weepy crusted lesions; itching, burning, stinging sensation; may pattern the area of contact
- Dx:
- clinical dx but bx if unsure
- Management:
- immediately wash the area with soap and water
- calamine lotion or oatmeal baths
- oral antihistamines or topical hydrocortisone cream
- oral corticosteroids depending on severity and area involved
- prevention of secondary infection

Digitalgadget at English Wikipedia / Public domain
Dermatitis Medicamentosa
Dyshidrotic Eczema
- Presentation:
- -F>M, 2:1
- -seen in patients with history of asthma or hay fever, patients whose hands are in constant hydration; “Tapioca” colored vesicles on palms/soles with pruritis; chronic, relapsing vesicular eczema; vesicles dry out/rupture and become scaly/fissured
- Management:
- -treatment with topical corticosteroids is more appropriate than with systemic corticosteroids
- treat pruritis with anti-histamine
Epidermal necrolysis
- Presentation:
- -lesion: small blisters on dusky pruritic macules (not seen in EM)
- mucosal involvement common
- prodrome of fever and malaise common
- -fever (often>102F) and flu-like illness 1-3 days before mucocutaneous lesions appear
- confluent erythema
- facial edema or central facial involvement
- lesions are painful
- skin necrosis, blisters, and/or epidermal detachment
- mucous membrane erosions/crusting, sore throat
- visual impairment (secondary to ocular involvement)
- rash 1-3 weeks after exposure, or days after 2nd exposure
- Steven johnson syndrome (similar in appearance to EM major):
- rare areas of confluence; detachment <10% BSA)
- Toxic epidermal necrolysis:
- confluent erythema common; outer layer of epidermis separates easily from basal layer with lateral pressure; large sheet of necrotic epidermis often present; >30% BSA involvement
Erythema Infectiosum
- Presentation:
- -fifth disease; slapped cheek syndrome; parvovirus B19; ages 5-15; outbreaks in close quarters
- Associated with:
- -arthritis: affects small joints of hands, occasionally ankles, knees, and wrists, symmetrical distribution
- -pregnant women: infection in 1st trimester has been linked to hydrops fetalis and miscarriage
- Transmission:
- via aerosol droplets/respiratory secretions; incubation time is 4-21 days
- Physical Exam:
- -low grade fever, headahce, and coryza; butterfly shaped maculopapular rashes on cheeks; rash may extend across nose and around mouth; lacy red rash may appear on torso and upper arms and legs; more confluent on the extensor surfaces; rash is rarely pruritic; lasts 2-4 days
- Dx:
- -clinical dx; PCR or ELISA for antibody testing
- Management:
- -treatment: supportive care

Andrew Kerr / Public domain
Erythema multiforme
- Presentation:
- -self-limited type IV hypersensitivity reaction
- -can be secondary to drug reactions, mycoplasma, or herpes simplex infections
- -minor: typically post-infectious pattern, most commonly HSV
- -major: <10% BSA involvement; commonly associated with medication use; may be associated with mycoplasma pneumonia; must involve at least two mucocutaneous surfaces; epidermal detachment; more systemic symptoms
- Physical Exam:
- -bull’s eye papules; extremities, face, lips (usually symmetrical); accompanies by fever, malaise, and arthralgia
- Management:
- corticosteroids
- Tylenol
 “Jack with Erythema multiforme” by jinglejammer is licensed under CC BY-SA 2.0
“Jack with Erythema multiforme” by jinglejammer is licensed under CC BY-SA 2.0
Erythema nodosum
Exfoliative dermatitis
- Presentation:
- -scaling of the skin that encompasses more than 30% BSA
- -can be secondary to: carcinoma (leukemia, lymphoma), systemic drugs (PCN, phenytoin, INH, barbituates, sulfa)
- Physcial Exam:
- -itching, weakness, malaise, fever, weight loss, loss of hair/nails, but spares mucosal membranes
- Dx:
- -clinical dx
- skin biopsy to show specific inflammatory dermatitis
- Management:
- topical with mid-potency corticosteroids
- stop offending agents
- systemic corticosteroids
Hand foot and mouth
- Presentation:
- -coxsackie virus
- Transmission:
- through nasal and pharyngeal secretions, saliva, vesicular fluid, and stool highly contagious, most infectious the first week of symptoms
- Physical Exam:
- -fever and stomatitis, sore throat and malaise 1-2 days, LAN (cervical and submandibular)
- oral lesions (apthae like); cutaneous lesions appear <24 hrs after oral lesions
- -3-7 mm red macules that progress into white vesicles with erythematous rings (“square blisters”); palms, soles, dorsal toes and fingers; less likely on face, buttocks, and legs 7 days to heal
- Dx:
- -clinical dx
- virus culture of fluid from vesicles
- negative tzanck smear
- Management:
- -mild and self-limiting
- tylenol for fever and pain control
- acyclovir suspension for patients 9 months-5 years of age if immunocompromised
 “File:Hand Foot & Mouth Disease.png” by BruceBlaus is licensed under CC BY-SA 4.0
“File:Hand Foot & Mouth Disease.png” by BruceBlaus is licensed under CC BY-SA 4.0
Lichen planus
- Presentation:
- -inflammatory and pruritic conditions with distinctive papules and insatiable pruritis
- -predilection for flexural surfaces
- -three cardinal features: characteristic skin lesions, mucosal lesions, infiltration of lymphocytes in the upper dermis
- -characteristic lesion: violaceous, flat, agulated papules with very fine white streaking; mucosal lesions have a lacy/reticular pattern; bx may reveal mononuclear cells with T cell mediated cytotoxic reagant against basal keratinocytes
- –the 5 P’s: pruritic, planar, polygonal, purple, papules
- Management:
- -treatment: high potency topical corticosteroids if localized; systemic corticosteroids in patients with acute systemic flares
- Prognosis:
- acute on chronic flares
- may lead to neoplastic changes in tissues in chronic
Lichen simplex chronicus
Measles
- Presentation:
- -high fever; Koplik’s spots; malaise; loss of appetite; coryza, hacking cough, conjunctivitis
- -rash develops 2-3 days after symptoms; starts behind ears and wraps around to the head and face, then proceeds to the rest of the body; generalized maculopapular, erythematous rash; may be pruritic; changes colors from red to dark brown before disappearing; usually lasts 6-8 days
- Dx:
- reportable to local health department; blood and throat/nasopharyngeal swabs for detection of measles-specific IgM antibody and measles RNA by real-time polymerase chain reaction (RT-PCR)
- Management:
- supportive care
- Prevention:
- MMR vaccine
- Complications:
- bacterial skin infection, otitis media, pneumonia, encephalitis, corneal ulcerations
- Risk factors:
- immunocompromised, unvaccinated people

CDC/NIP/Barbara Rice / Public domain
Molluscum Contagiosum
- Presentation:
- -caused by poxvirus; peak age is around 3-9 years and 16-24 years; commonly affects immunocompromised patients
- Transmission
- via contact and autoinoculation; lesions spread along inflamed skin
- Physical Exam:
- -1-2 mm shiny, white flesh colored, dome shaped firm papules; children = upper trunk, extremities, face; young adults = usually STI; lower ab, thighs, and pubic region; papules become softer and pink in color with central umbilication
- Dx:
- -biopsy = molluscum bodies with infected keratinocytes; curettage = express white rubbery core of papule that can be used on KOH prep
- Management:
- -keep covered to decrease spread;
- curettage cryosurgery
- kids = cantharidin 0.7% solution with occlusive dressing
- adults = topical tretinoin for 1+ month
- untreated may last 6-9 months
 “File:Molluscaklein.jpg” by E van Herk is licensed under CC BY-SA 3.0
“File:Molluscaklein.jpg” by E van Herk is licensed under CC BY-SA 3.0

Gzzz / CC BY-SA
Mumps
- Presentation:
- -spring and winter months; outbreaks in confined populations; young adults
- Transmission:
- via aerosol droplets, respiratory secretions, virus can survive on external surfaces
- Phsyical Exam:
- -fever, headaches, malaise, anorexia, dry mouth and sore face/ears are prodromal sxs; painful swelling of salivary glands, specifically parotid gland (“hamster cheeks”);orchitis (15-20% of post-puberty males)/oophoritis
- Dx:
- PCR of saliva and blood for antibody testing; serum amylase to R/O pancreatic involvement
- Management:
- -warm compress; soft foods, saltwater gargles; pain medications
- Vaccine:
- -MMR vaccine: live attenuated virus; two doses (12 months, 4-6 years)
- Complications:
- infertility/subfertility in males; meningitis; pancreatitis
- Risk factors:
- unvaccinated patients; highly populated close quarters
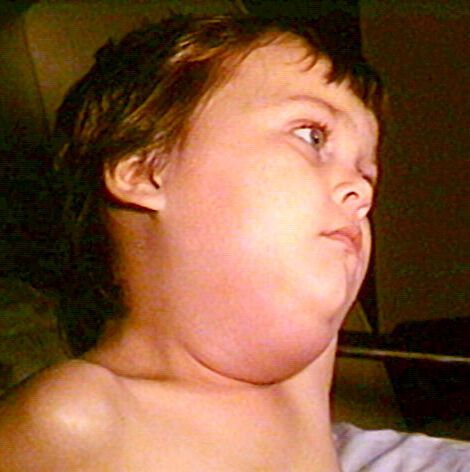
Photo Credit:Content Providers: CDC/NIP/Barbara Rice / Public domain
Photodermatitis
Rosacea
- Presentation:
- -unclear etiology but secondary to chronic vasomotor instability which leads to permanent vasodilation and lesion formation; W>M, more common in celtic population; usually occurs in 30s-50s
- -facial flushing with increase in temperature or with consumption of ETOH
- Pathophysiology:
- increase reactivity of facial capillaries leads to flushing and development of telangectasia; dilation of superficial capillaries leads to perifollicular inflammation that causes papules and pustules
- Physical Exam:
- -symmetric erythema of the face; telangectasia; pustules and central facial edema
- Dx:
- skin biopsy helpful for staging
- Management:
- topical antibiotics, systemic antibiotics
- isotretinoin (retin A) for severe cases
- clonidine
- avoidance of provocative factors
Roseola Infantum
- Presentation:
- -children b/w 6 months-1 year; caused by HHV-6
- fall and spring epidemics
- incubation period = 5-15 days
- Transmission:
- via respiratory droplets and oral secretions
- Physical Exam:
- ~70% of patients are asymptomatic sudden high fever (>103F) for three days
- after the fever subsides, a rose colored maculopapular rash appears
- usually begins on trunk, spreading to the legs and neck/face; the rash is not itchy and may last 1-2 days
- Management:
- supportive care
- Complications:
- febrile seizures
- immunocompromised (pneumonia, encephalitis)

Emiliano Burzagli / Public domain
Rubella
- Presentation:
- -malaise, fever, and anorexia are prodromal; LAN (posterior auricular, cervical, and suboccipital)
- maculopapular rash that starts on the face and spreads down the body (lasts 3-5 days)
- Transmission:
- via aerosol droplets; virions are present on skin and in urine and feces
- Dx:
- can be difficult; PCR or ELISA for antibody testing
- Management:
- supportive care
- Prevention:
- MMR
- Associated with:
- Pregnant women:
- greatest risk is b/w 28 days before conception (increased risk of miscarriage) and 12 weeks after conception (congenital rubella)
- Congenital rubella syndrome:
- infants stay contagious for months
- sensorineural deafness (58%)
- eye abnormalities (43%-retinopathy, cataracts, micropthalmia)
- CHD (50%-pulmonary stenosis, PDA)
- microcephaly, hepatomegaly, blueberry muffin rash, autism, developmental delays, mental retardation
- Arthritis:
- mostly in women with fingers, wrists, and knees affected
- Pregnant women:

Photo Credit:Content Providers(s): CDC / Public domain
Urticaria
- Presentation:
- -IgE or complement mediated edema of the dermis and/or subcutaneous tissues
- -may be idiopathic, hereditary, or caused by insect bites, medications, exposures to head/cold
- -mast cells are stimulated to degranulate; histamine leads to vasodilation which leads to edema
- -blanchable, pink, edematous papules or plaques; these lesions may colaesce; acute – typically resolves within 24 hours
- Dx:
- -clinical dx
- persistence may require further testing
- Management:
- eliminate causative factors
- H1/H2 blockers
- mast cell stabilizers
- steroids topical, oral, IM, or IV depending on severity
 “File:Urticaria child.jpg” by Gzzz is licensed under CC BY-SA 4.0
“File:Urticaria child.jpg” by Gzzz is licensed under CC BY-SA 4.0
Varicella Zoster
- Presentation:
- -virus; respiratory droplets
- -rash begins as small red dots on the face, scalp, torso, upper arms and legs; progressing over 10-12 hours to small bumps, blisters and pustules; followed by umbilication and the formation of a scab; low grade fever; malaise; “dew drops on a rose petal
- Dx:
- -tzank smear; IgM and IgG
- Management:
- treat fever and supportive care
- antivirals, vaccine, nerve block
- narcotics
 “File:Chicken Pox (Varicella Zoster).jpg” by BruceBlaus is licensed under CC BY-SA 4.0
“File:Chicken Pox (Varicella Zoster).jpg” by BruceBlaus is licensed under CC BY-SA 4.0
Verrucae Vulgaris
- Presentation:
- -caused by HPV; transmission via contact and autoinoculation
- peak age =12-16 yo; incubation period = 1-6 months
- -flesh colored papules that evolve into dome shaped gray brown, hyperkarytotic growth with black dots on surface (thrombosed capillaries)
- common sites include hands, feet, elbows, knees, and genitalia;
- HPV-1 = palmar and plantar warts; HPV-2 = common warts; HPV-3 and 10 = flat warts
- Management:
- -usually spontaneous resolution
- sometimes treatment can be difficult
- OTC topical salicyclic acid daily
- liquid nitrogen cryotherapy Q2-3 weeks
- electrocautery, laster surgery








