Gram Positive Bacteria section provides High Yield Information needed for USMLE, COMLEX, Medical School, Residency, and as a practicing Physician.
Table Of Contents

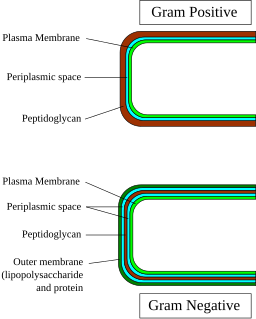
Huckfinne / Public domain

LadyofHats / Public domain
Cocci
Enterococcus

Photo Credit:Content Providers(s): CDC/Dr. Mike Miller, Public domain, via Wikimedia Commons
- Features:
- Gram-positive cocci
- Normal flora of intestines
- 2 Species: E faecalis – most common, E faecium- less common more serious infections
- Grows in 6.5% NaCl
- Bile resistant
- Causes:
- – UTI
- – Endocarditis
- – Biliary tree infection
- Types:
- E faecium
- Most common species
- Nosocomial infection that is resistant to almost every antibiotic
- Causes: VRE vancomycin-resistant enterococcus
- Treatment:
- Linezolid: IV antibiotic
- Tigecycline
Staph Aureus

Content Providers(s): CDC/ Matthew J. Arduino, DRPHPhoto Credit: Janice Haney Carr, Public domain, via Wikimedia Commons
- Features:
- Gram-positive cocci in clusters
- Beta-hemolytic
- Coagulase-positive
- Catalase-positive
- Ferments mannitol
- Colonizes the nares
- Virulence factor: protein A binds to IgG
- TSST-1:
- Causes:
- TSST causing toxic shock syndrome
- Exfoliative toxin causing scalded skin syndrome
- Fast-acting food poisoning (preformed)
- Post-viral upper respiratory pneumonia
- Tricuspid endocarditis in IV drug users
- Osteomyelitis
- Septic arthritis
- Abscess
- Pneumonia: patchy lung infiltrate on CXR
- Alterations in penicillin-binding proteins–> resistance (MRSA)
- Treatment of choice:
- Nafcillin
- Vancomycin for MRSA
Staph Epidermidis
- Features:
- Gram positive cocci in cluster
- Normal flora in skin
- Catalase positive
- Coagulase negative
- Urease positive
- Novobiocin sensitive
- Associated with prosthetic valve, prosthetic joint and catheter infections produces biofilm that adhere to prosthetic surfaces
- **Most common cause of endocarditis affecting implanted/prosthetic valves
- Treatment:
- Vancomycin
Staph Saprophyticus
- Features:
- Gram positive cocci in cluster
- Normal flora
- Catalase positive
- Coagulase negative
- Novobiocin resistant
- Commonly infects sexually active women
- **Most common cause of UTI in sexually active women**
- Gram positive cocci in cluster
- Treatment:
- Vancomycin
Strep Pneumonia
- Features:
- Gram-positive diplococci lancet-shaped
- Alpha hemolytic – partial hemolysis
- Encapsulated: polysaccharide = major virulence factor
- Protease cleaves IgA- allows colonization and invasion of the mucosa
- Optochin sensitive
- Bile soluble
- Causes:
- MOPS: meningitis, otitis media, pneumonia, sinusitis
- Pneumonia- with rusty sputum
- Higher risk patients
- Post-splenectomy due to encapsulated bacteria
- Treatment:
- Erythromycin or Ceftriaxone
- Vaccination:
- Adult: 23 valent polysaccharide- IgM
- Children: 7 valent polysaccharide conjugated- IgG
Strep Viridians
- Features:
- Gram positive diplococci
- Alpha hemolytic
- Optochin resistant
- Bile resistant
- Types:
- Strep Mutans: causes: Mostly dental caries
- Strep Sanguinus: infects blood : endocarditis in previously damaged heart valves. Adheres to fibrin platelet aggregates in damaged heart valves. synthesizes dextrans from glucose
Strep Pyogenes (Group A Strep)
- Features:
- Gram-positive cocci in chains
- Beta-hemolytic
- Bacitracin sensitive
- Encapsulated: hyaluronic acid capsule
- Streptolysin O:
- Exotoxin A:
- Causes:
- Pyogenic infections:
- Impetigo
- Pharyngitis
- Cellulitis and erysipelas (Strep pyogenes: most common cause of erysipelas)
- Streptococcal pyrogenic exotoxin/SPE
- Scarlet fever
- Toxic shock-like syndrome
- Necrotizing fasciitis
- Rheumatic fever
- Type II hypersensitivity: M protein in the cell wall. AFTER PHARYNGITIS
- JONES Criteria:
- J = Migratory polyarthritis (J stands for joints!)
- O = Carditis (O shaped like a heart!)
- N = subcutaneous Nodules (N stands for Nodules!)
- E = Erythema marginatum (rash) (E stands for Erythema!)
- S = Sydenham chorea (S stands for Sydenham!)
- Post strep GN
- Two weeks after the initial strep infection
- Streptolysin O – generates ASO
- Treatment:
- Penicillin
Strep Agalactiae (Group B Strep)
- Features:
- Gram positive cocci in chains
- Encapsulated with polysaccharide capsule
- Beta hemolytic
- Bacitracin resistant
- Hydrolyzes Sodium Hippurate
- Positive CAMP test – enhances hemolysis by staph aureus
- Causes:
- Very serious infections in newborns
- Sepsis in newborn
- Meningitis in newborn
- Pneumonia in newborn
- Very serious infections in newborns
- Treatment:
- Treat mother with group B strep infection by 35 week AOG–> Intrapartum penicillin
Rods
Bacillus anthracis
- Feature:
- Gram-positive rods in chains
- Encapsulated- protein (poly-D glutamate)
- Obligate aerobe
- Spore former
- Toxins: Lethal factor and Edema factor
- Edema Toxin (Edema Factor):
- Causes:
- Black escar
- Pulmonary anthrax / Woolsorter’s disease
- Inhalation of spores- nonspecific symptoms, mediastinal LN-> hemorrhagic mediastinitis. CXR: widened mediastinum
- Treatment:
- Early detection
- DOC Fluoroquinolones
- Doxycycline
Bacillus cereus
Clostridium botulinum

Content Providers: CDC, Public domain, via Wikimedia Commons
Clostridium difficile
Clostridium perfringens
- Features:
- Gram-positive rod Club shaped
- Diphtheria
- Exotoxin–> cell death–> formation of pseudomembranes- thick yellow exudate over the mucosal surface of the oropharynx
- Diphtheria toxin:
- Commonly seen in:
- Immigrants
- Causes:
- Pseudomembranes in throat and trachea
- Lymphadenopathy/Bull’s neck
- Myocarditis- life threatening
- Local paralysis
- Vaccination:
- Toxoid vaccine- inactivated exotoxin conjugated to protein
- Treatment:
- Passive immunization/IG
Clostridium tetani
Corynebacterium diphtheriae

Photo Credit:Content Providers(s):, Public domain, via Wikimedia Commons
- Features:
- Gram-positive rod
- Spore forming – found in dirt and soil
- Obligate anaerobe
- Double zone of hemolysis
- Alpha Toxin:
- Classic Presentation:
- Motorcycle accidents
- Deep penetrating wounds
- Long term exposure of a large amount of flesh to dirt and dust
- Clinical Presentation
- Gas gangrene / Clostridial myonecrosis
- Food poisoning- a large number of spores
Listeria monocytogenes

Elizabeth White, Public domain, via Wikimedia Commons
- Features:
- Gram positive rod
- Beta hemolytic
- Motile
- Facultative intracellular
- Catalase positive
- Survives in near freezing temperatures
- Commonly seen in:
- Unpasteurized milk
- Packaged meat
- Soft cheeses
- Pregnant women – most susceptible to infection
- Early pregnancy- early termination
- Late pregnancy- disease in newborn
- Causes:
- Newborn meningitis
- >60 years – meningitis
- Treatment:
- Adult meningitis: Vancomycin and Ceftriaxone
- Elderly meningitis: Vancomycin, Ceftriaxone, and Ampicillin
- Listeria: Ampicillin
Filamentous/Branching Rod
Actinomyces
- Feature:
- Gram positive filamentous rod/Branching rod
- Obligate anaerobe
- Normal flora of oral cavity
- Classic presentation:
- Dental procedure: Cervicofacial actinomycosis infection:
- Infection associated with jaw trauma- infection spreads to head and neck- invades surrounding tissue
- Actinomyces infection:
- Slow course- non-tender lump on jaw then forms abscess. sinus tract appears and drains infection site through the skin
- Yellow thick pus -yellow sulfur granules
- Dental procedure: Cervicofacial actinomycosis infection:
- Treatment:
- Penicillin
- If complicated: surgical drainage
Nocardia
- Feature:
- Nocardia asteroides
- Gram positive filamentous/branching rod
- Obligate aerobe
- Found in soil primarily
- Catalase positive
- Urease positive
- Seen commonly in immunocompromised patients:
- Impaired cell mediated immunity
- HIV
- Transplant patients
- Patients taking glucocorticoids
- Men > women
- Infection in 3 sites: Pulmonary, CNS, Cutaneous
- Lung abscess. associated with cavitary lesions in lung – able to disseminate
- Brain abscesses- high affinity to neural tissue
- Open wound exposed to dirt–> pyogenic response
- Treatment:
- Sulfonamide
Gram Positive Bacterial Quiz 1
3